Unitary Manifold, a branched PMEG with a 8 years experience.
- Nov 5, 2024
- 6 min read

Today, we have the privilege of interviewing Dr. Patrick Kelly, a vascular surgeon based in Dakota, USA. Dr. Kelly and his team have recently published an article on the mid-term follow-up of 126 patients treated with his surgeon-modified Unitary Manifold prosthesis.

Additionally, he and his team hold 66 patents and have conducted numerous studies on the treatment of thoracoabdominal aneurysms. In addition to this interview, you can view a detailed explanation of its assembly on this same website (see the 'How to Do It!' section). Let’s dive into the details of the Unitary Manifold!
Javier Río: The results of this device are exceptional, with very low rates of neurological complication or branch thrombosis. It is noteworthy to achieve these results with branch strategies that involve greater aortic coverage and longer bridging stents. What do you think is the reason for this?
Patrick Kelly: Thank you. When I started this project, I honestly expected the outcomes that we are seeing. There is a Mark Twain saying that comes to mind and I think might apply here. “Its not what you don’t know that gets you in trouble. It’s what you know that isn’t so that does.”

I think there are some big misnomers here. Assuming Branch Devices are going to have a higher branch occlusion rate then Fenestrated Devices just because the branches are longer might not be right. If bridging stent length was the only factor effecting occlusion rates, this might be true, but I don’t think it is.
You might remember my background is in Engineering, so I always look at problems from a root cause effect. If we look at the flow dynamics around the branches we have to consider the inflow to the branches (how disrupted is the blood flow entering the bridging stent), the branch diameter (flow is based on radius to the 4th power so diameter is a real consideration), wall resistance (how smooth vs how rough is the pipe), the path of the pipe (straight or turns) and the outflow. Basically the same rules we follow when doing a bypass.

We looked at these very issues with CFD modeling of the different stent graft configurations. We also looked at some new variable called near-wall hemodynamics.
Near-wall hemodynamics looks at blood flow along the wall of the vessel. The theory here is that if blood flow is not laminar or undeveloped the blood along the vessel wall is not moving. If this is the case, then the blood suppling the endothelial cells isn’t being refreshed.
In otherwards the endothelial cells are not seeing fresh re-oxygenated blood at a needed rate causing endothelial cell ischemia and inflammation (intimal hyperplasia). This would explain the reason we see such low occlusion rates with the Unitary design.
Our branches are slightly long and we cover a little more aorta but because of our design we see very little disruption of blood flow entering our branches, our gradual sweeping branches allow time for that blood flow to re-organize (become laminar) again and by the time the branch blood flow come into contact with the native vessel it is fully re-organize providing a normal hemodynamic flow state to the visceral and renal arteries.
Here are some hyperlinks to the papers I have referenced. https://pubmed.ncbi.nlm.nih.gov/26209577/
With regards to low SCI events, I think the Unitary Manifold might not be covering as much aorta as is appears. The Top of the Unitary Manifold main body is 8-9cm above the celiac artery. This is very similar to the other current grafts. We also set a post operative management protocol that other sites have implemented with similar SCI event rates. It all comes down to fluid management and tissue perfusion. We only use spinal drains for rescue situations that we’ve had to use less then 3 times with success in all but one two patients. We published a paper around our management protocol.

JR: Regarding the creation of the device, how long does it take to develop? Is the length of the branches always the same? Does any detail of the device configuration change depending on the anatomy, or could we speak of a device that could be “off the shelf”?
PK: If I am understanding your question correctly. It takes me about an hour and 10 minutes to assemble the Unitary Manifold. This being said I’ve assembled about 250 plus graft from our first generation Manifold to the Branch Iliac graft to finally the Unitary Manifold. Other Physicians that have assembled the Unitary Manifold will tell you the first few times it takes about 2 hours to assemble but with experience that time is cut drastically to an hour and 20 to an hour and 30 minutes.
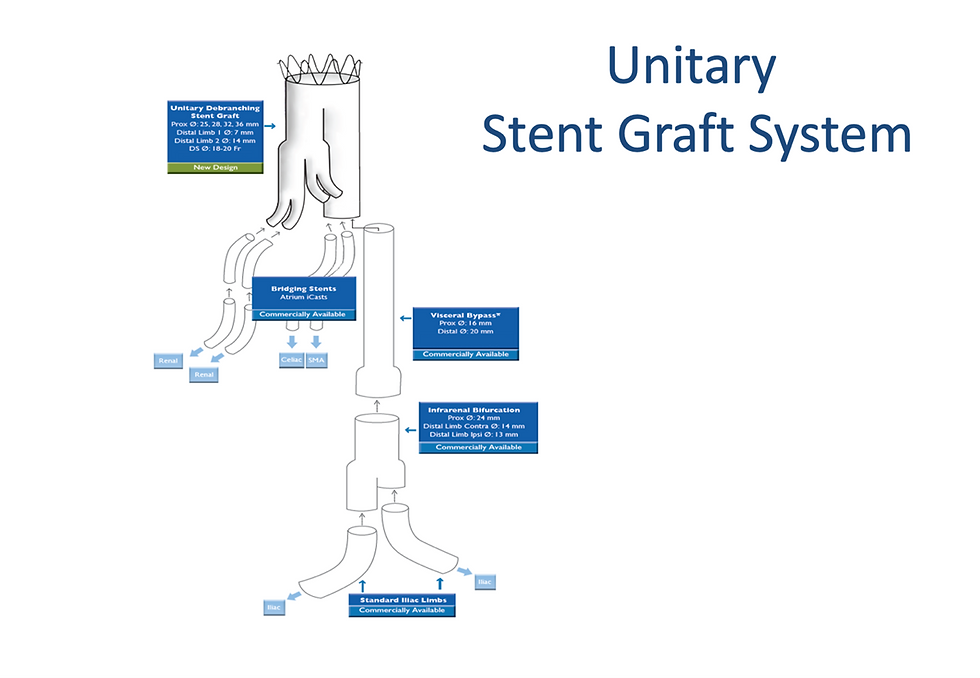
In our recent publication of 126 patients, we assemble the graft the same each time. I think this plays into why we can assemble the graft so efficiently. My self and the staff know how to put this graft together. We can do it without saying a single word. Its built independent of the patient’s anatomy except the diameter of the Endurant we use. Its either a 28/32 or 36 Endurant from there they are all the same. With regards to limb length the Celiac Limbs is assembled from a 7mm x 2.5cm Viabahn, the SMA is from 8mm x 5cm Viabahn cut down to 3cm in length while the renal branches are assembled from 2-7mm x 5cm Viabahn cut down to 3cm.
JR: The Endurant delivery system is designed for the Abdominal Aorta and is not very long. Have you encountered any issues where you couldn’t reach proximal enough in the thoracic aorta? Could this be a limitation in taller patients?
PK: We have not encountered this problem since moving to the Unitary Manifold device. Keep in mind we are actually only deploying the Unitary Manifold about 15 cm or 6 inches above the renal arteries. Obvious there might be someone so tall that this might be a limitation but after 200+ patients at several different sites we have not yet encountered this.
JR: Our readers surely have this question in mind. At a time when commercial “off the shelf” prostheses such as TAMBE, T-Branch, or Enside are available on the market, what advantages does the Unitary Manifold device offer? What would its limitation be?
PK: The Unitary Manifold is a very different design. It is a nonanatomical design. With the 3cm mobile limbs we have found that this graft configures to the patients anatomy verses trying to either custom figure the graft to the patients anatomy ie fenestration or force a fixed graft configuration to a patients anatomy… This might explain the high bridging stent occlusion rates we are seeing in branch systems. TAMBE in their pivotal trial had a 15% branch occlusion rate. The other limitation that has continued to bear out in the literature is T-branch, Enside and most likely TAMBE can only fit about 50% of the presenting anatomy. Our recent paper showed how the Unitary Manifold performed in 126 consecutive patients with no screen failures and a greater then 99% technical success.
I think the Unitary Manifold biggest limitation is Perception. The branches are to long so we will see higher occlusion rates… We actually see lower occlusion rates and lower reintervention rates. Super Celiac coverage is to much thus will see high SCI events. We haven’t. We have seen a less then 2% paraplegia rate. It’s not perfect and I think it can be better but all of these results a reasonable for the patient population we have treated.
Other limitation is requiring arm access to deliver bridging stents. Fortunately, because we are able to treat one visceral/renal stent at a time we are able to use a 8.5Fr directional sheath from a small brachial cutdown.
JR: If you could change one characteristic of the commercial prostheses to make its modification easier, what would it be?
PK: I’m not totally sure Im following the question. If you are asking about modifying the Unitary Manifold. Understand this is our next generation device. I honestly wouldn’t change much. Its flow dynamics are very good and its usability is really good. I am working on a 3rd generation device but obviously from a patentability standpoint I can’t say much.
JR: Finally, how do you see the future of endograft modification by physicians? Do you believe it would be feasible to have a scenario in the short-to-mid term where we have prostheses that can be modified according to certain guidelines, while still adhering to the instruction for use (IFU).
PK: Terumo and Dr Starnes are working on this very option. I think the more feasible scenario is a prostheses that is an Off-The-Shelf design that will fit virtually any anatomy with favorable outcomes… Oh I just described the Unitary Manifold Stent Graft System. We just need a partner to commercialize it.
Thank you very much, Dr. Kelly. I’m sure the readers are pleasantly surprised by all the information you’ve shared with us in this interview.




Comments